Interpreting excess mortality in England: week ending 9 October 2020
October 23, 2020
Carl Heneghan, Dan Howdon, Jason Oke, Tom Jefferson
Summary:
Excess deaths remain low in England, with 112 observed in the most recent week reported – one percent higher than expected. Across the regions, excess deaths do not show a consistent picture.
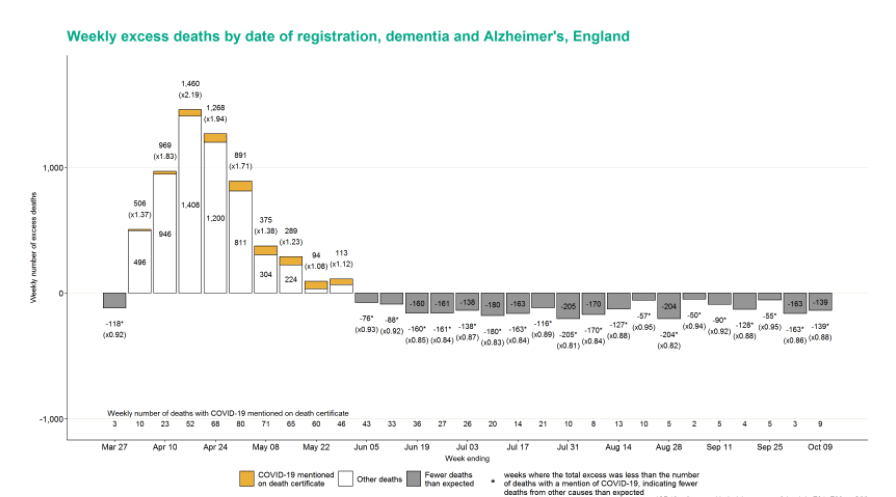
In terms of death by an underlying cause, ischaemic heart disease and stroke continue to show excess deaths, and diabetes mellitus has seen excess deaths in all 29 weeks of the PHE reporting window. In contrast, Dementia and Alzheimers have seen deaths lower than expected for 19 consecutive weeks with 139 (12%) fewer deaths than expected this week. There are also notably fewer deaths for chronic lower respiratory conditions, other respiratory conditions and acute respiratory infections.
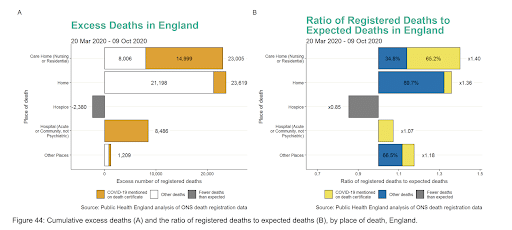
Deaths in own homes have seen an excess of 23,619 since week 14, a similar number to the 23,005 excess deaths in care homes. Both far exceed the excess noted in hospital. While the majority of COVID-19 deaths have occurred in hospitals (n=32,275), the excess is only 8,486 or 7% higher than what would be expected.
The deaths of people in their own homes are predominantly due to other causes: 2,421 (roughly 10%) are COVID-19 deaths. In care homes, COVID-19 deaths make up 65% of the excess (n= 14,999).
While the number of COVID-19 deaths may be high, particularly in the hospital setting, the analysis of excess deaths is a crucial consideration for assessing the impact of covid. The data suggest that mortality has shifted from hospital to home, especially for deaths not associated with COVID-19. This “displacement” may be due to the reluctance of individuals to receive treatment in hospital or of clinicians to admit non-covid patients.
The PHE methods use an estimate of the number of deaths we would expect on each day in 2020. This contrasts with the Office for National Statistics method, which uses a simple five-year average.
Conclusion: a significant amount of displacement has occurred that is reflected in the lower than expected deaths in older age groups and Alzheimer and dementia deaths through the summer. In-hospital deaths with a positive covid test are the highest for any setting; however, they contribute much less to the overall excess in deaths. Deaths in the home remain persistently high, and yet they receive little attention.
Link to PHE report:
Excess mortality allows an understanding of the impact of COVID-19. Each week Public Health England produces a weekly report that models the expected number of deaths using an average of five years of data, adjusted for factors such as the ageing of the population and the underlying trend in mortality rates from year to year. This is used to estimate the number of deaths we would expect on each day in 2020. This contrasts with the Office for National Statistics (ONS) method, which uses a simple five-year average.
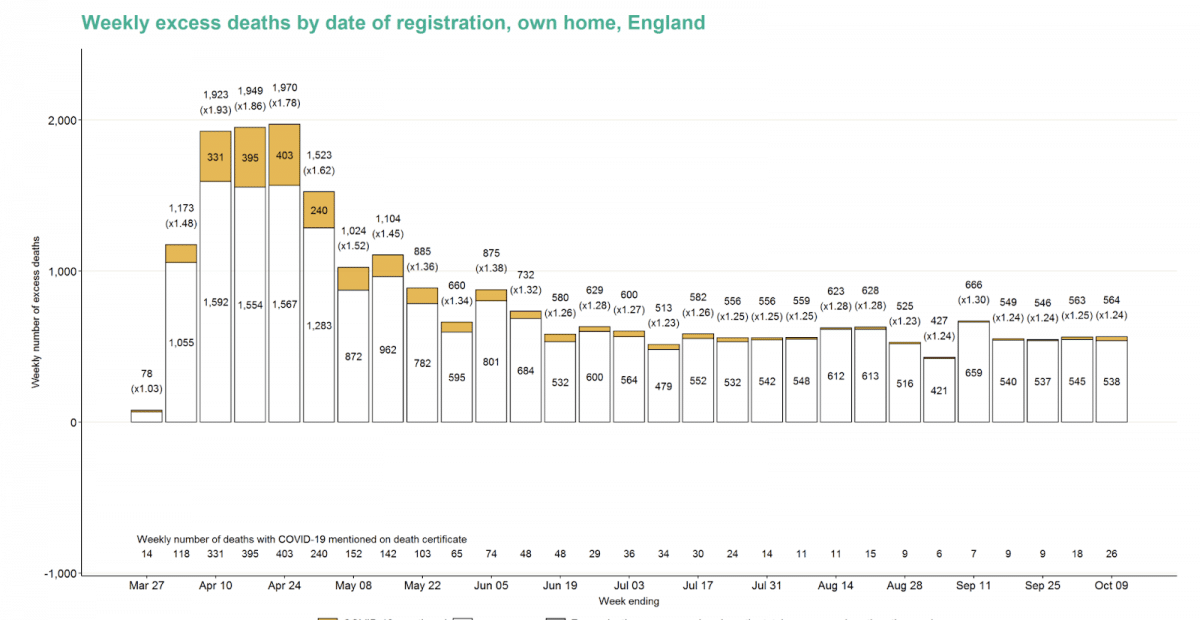
Weekly excess deaths by date of registration, England.
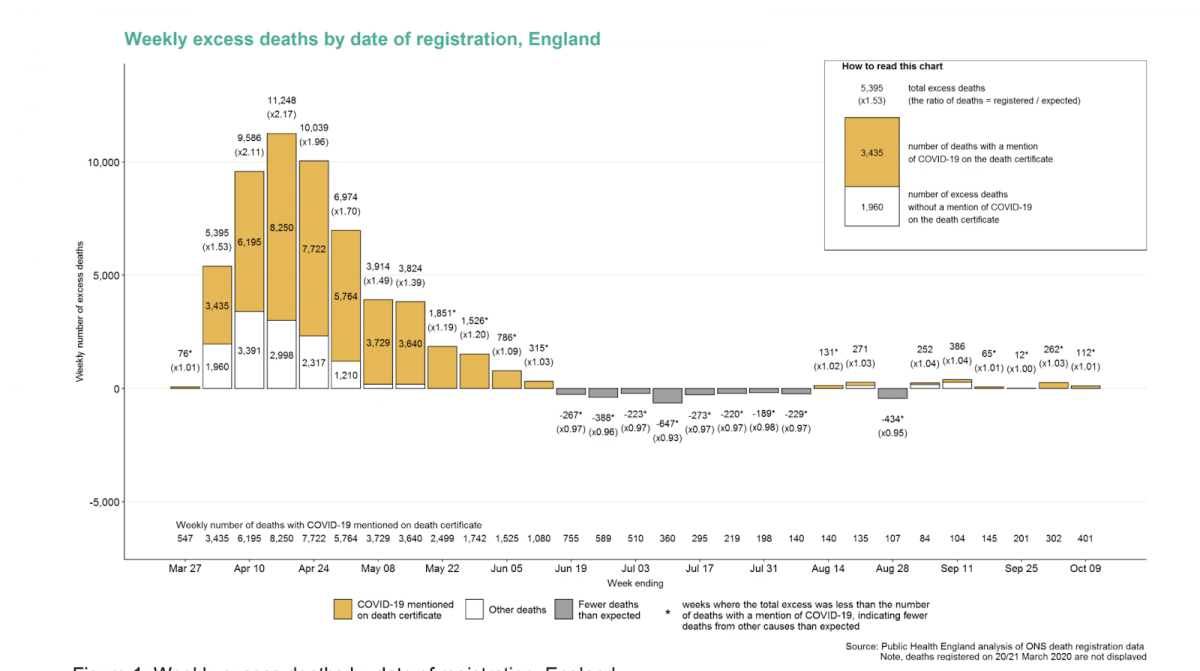
Excess deaths where COVID-19 was mentioned on the death certificate are shown in orange. In the week ending the 9 October, there were 112 excess deaths in England (1 percent higher than expected). For the same week, the ONS reports 140 excess deaths for England.
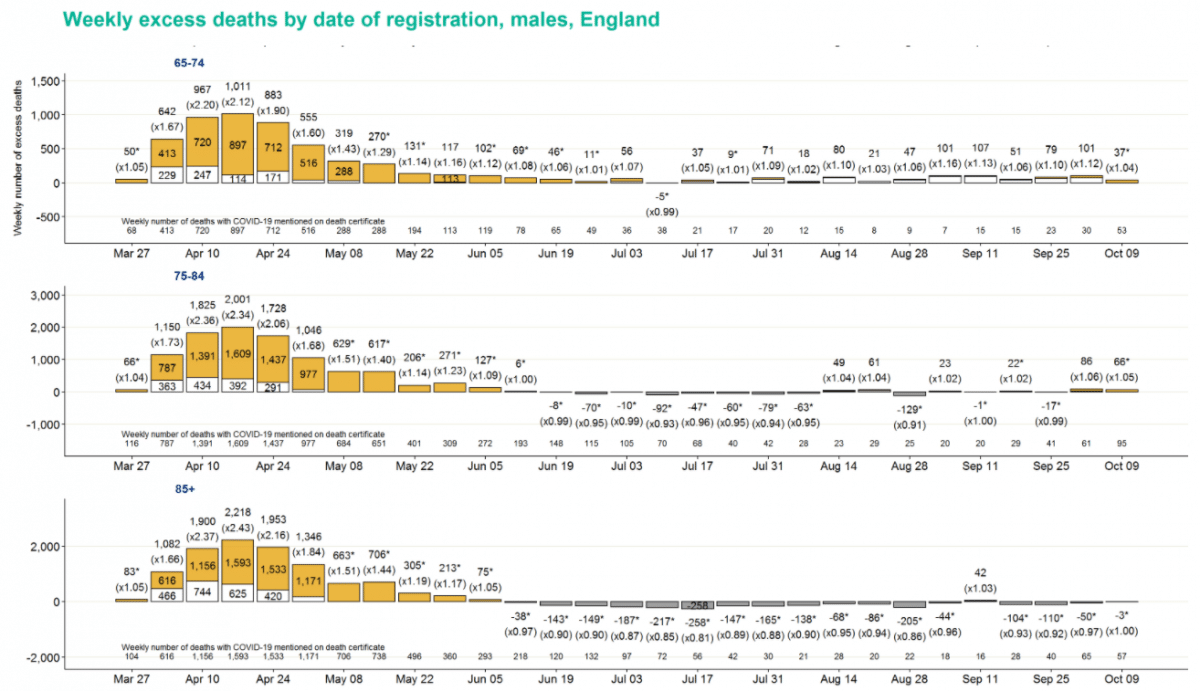
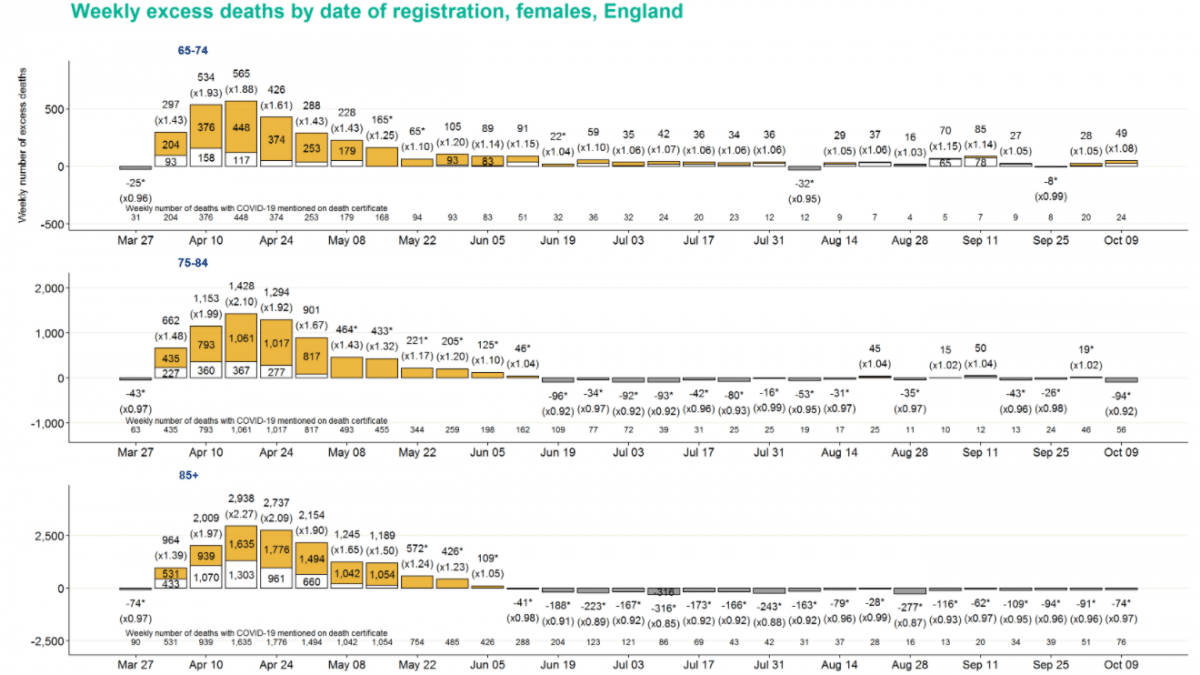
Deaths by age group
Notable levels of positive excess deaths – almost entirely not explained by death certificate mentions of COVID-19 (at levels well over 10% in most weeks) have been observed in the 15-44 and 45-64 age groups.

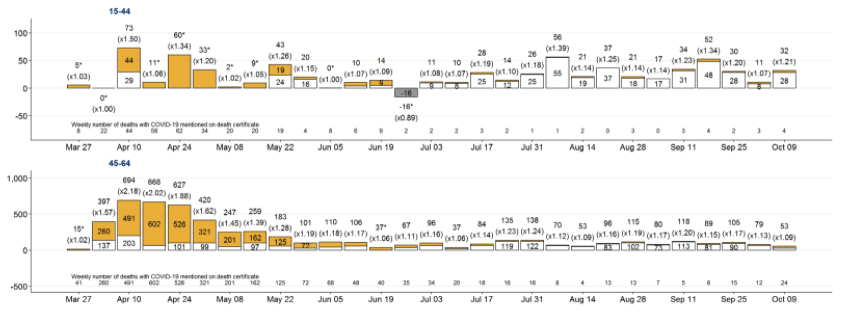
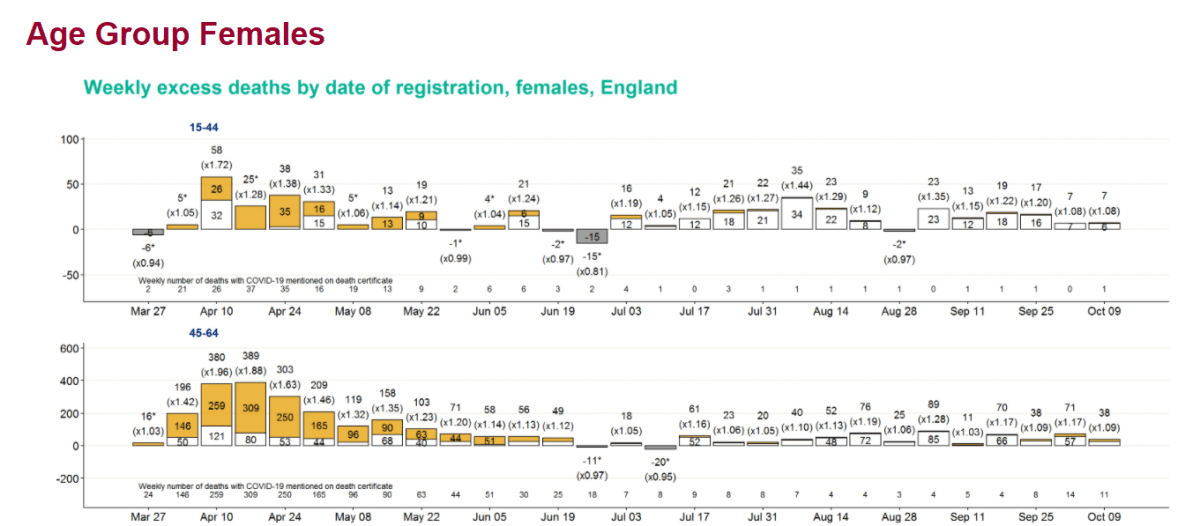
Conversely, levels of excess mortality in older age groups have generally been lower. Excess mortality for the over 85 age group has been negative for all bar one of the last 18 weeks for men, and all of the last 18 weeks for women.
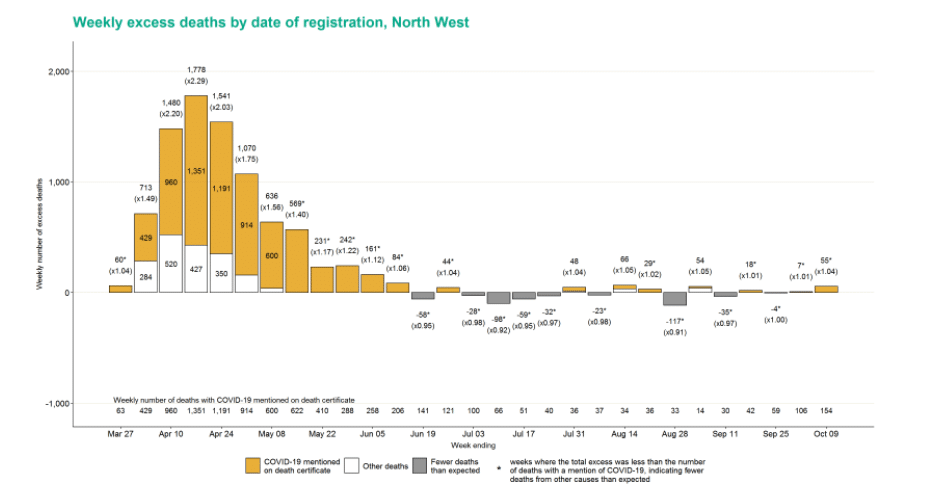
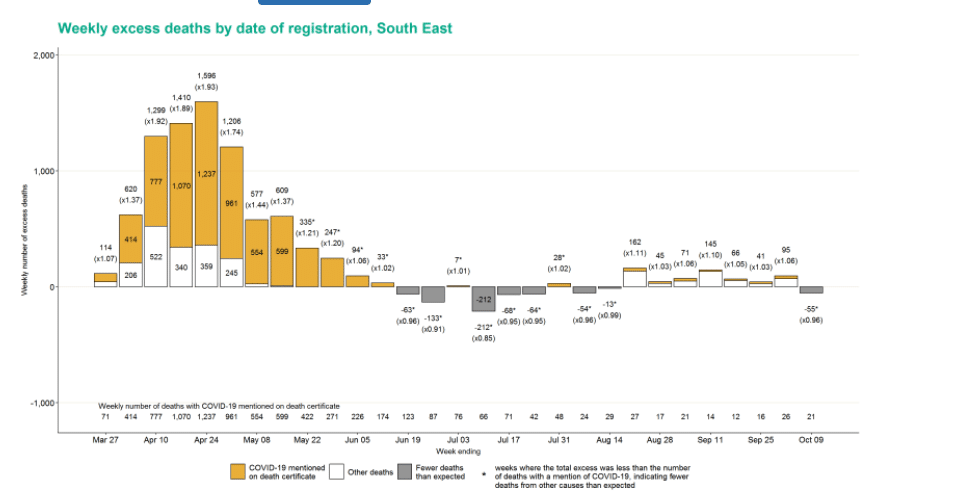
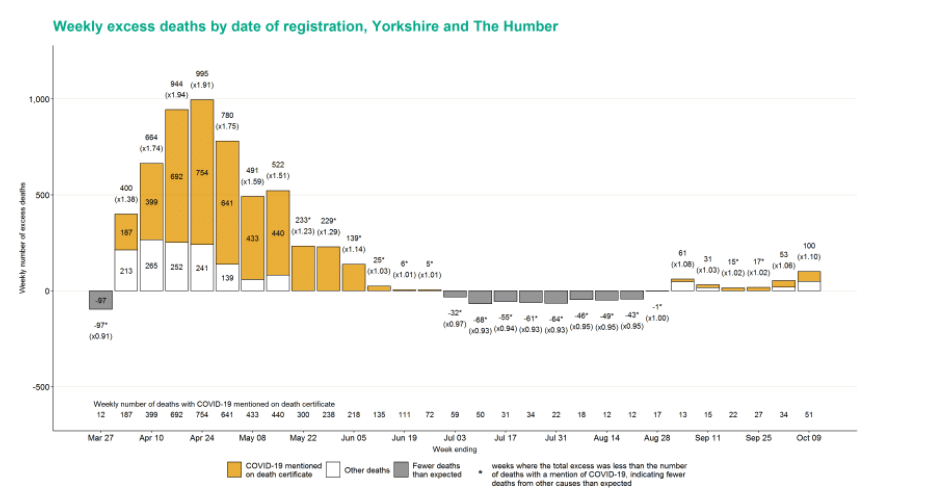
Deaths by region
Across regions, excess deaths do not show a consistent picture. In the North West, where COVID-19 deaths are highest, there were 55 (4%) excess deaths. In the South East where cases are one of the lowest, there is no pattern consistent with death certificate mentions of COVID-19: There have been seven weeks of excess deaths (n=625) followed by this week’s 55 fewer deaths than expected.
The Yorkshire and the Humber region saw the most excess deaths in week 42 with 100 (10%) more than expected.
Deaths by underlying cause
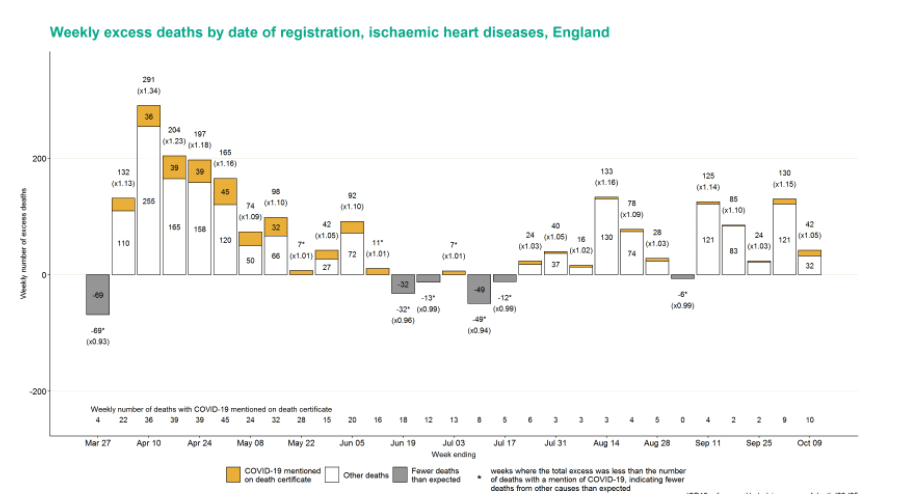
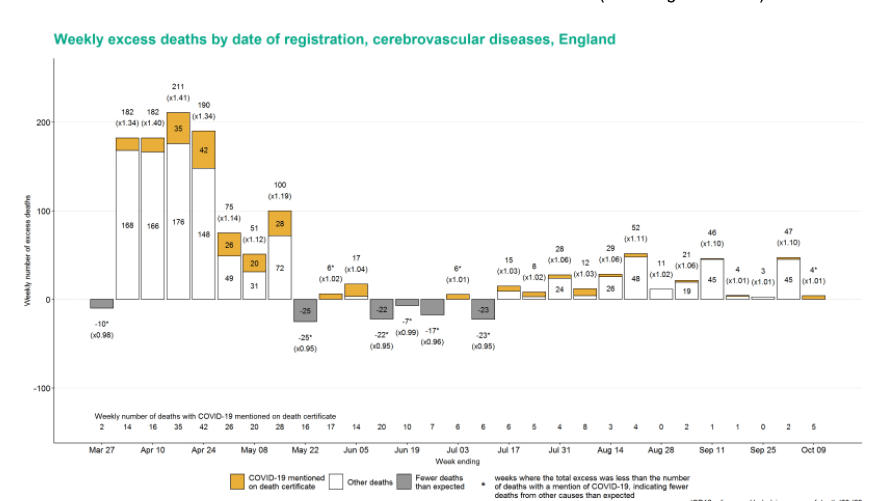
In terms of death by underlying cause, ischaemic heart disease (IHD) continues to shows an excess with 42 (5%) deaths higher than expected, and they have been in excess for 11 of the last 12 weeks. Stroke has also seen excess deaths for 13 weeks in a row.
In contrast, Dementia and Alzheimers have seen deaths lower than expected for 19 consecutive weeks with 139 (12%) fewer deaths than expected this week.
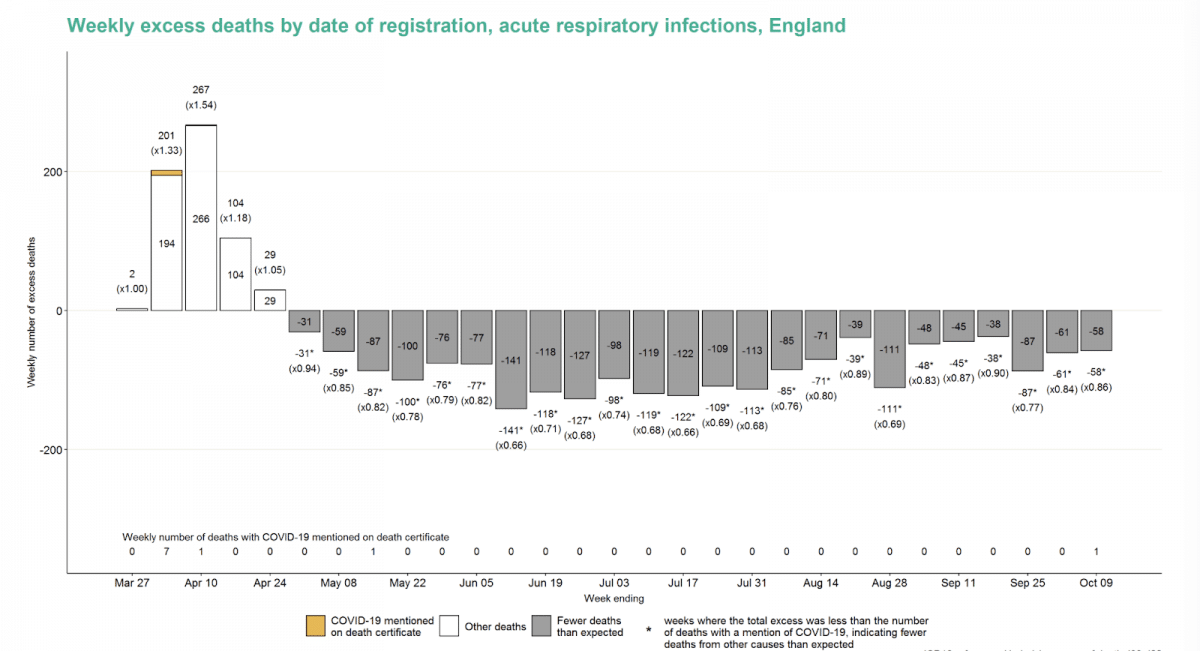
There were notably fewer deaths for chronic lower respiratory conditions; other respiratory conditions and acute respiratory infections.
In those deaths with a mention of specific causes, diabetes mellitus has seen excess deaths in all 29 weeks of the PHE reporting window. At the same time, influenza and pneumonia deaths have been lower than expected for the last 16 weeks.
Deaths by place of occurrence
Deaths in own homes have seen 23,619 excess deaths in the reporting window since week 14. This is a similar number to the 23,005 excess deaths in care homes that both exceed the 8,486 excess deaths observed in hospital.
Deaths in own homes are predominately due to other causes: 2,421 (roughly 10% of the excess) are COVID-19 deaths in their own homes. In care homes, the Covid deaths make up 65% of the excess (n=14,999). While the majority of COVID-19 deaths have occurred in hospital (n=32,275), the excess deaths are only 8,486 or 7% higher than expected.
The ONS similarly reports for the same week numbers of deaths in hospitals and care homes remaining below the five-year average (374 and 175 fewer deaths respectively). In comparison, the number of deaths in private homes remained 705 above the five-year average in the ONS report.
The data suggest that mortality has shifted from hospital to home, especially for deaths not associated with COVID-19. This “displacement” may be due to the reluctance of individuals to receive treatment in hospital or of clinicians to admit non-Covid patients or a combination of these.
Daniel Howdon is a Senior Research Fellow in Health Economics, Leeds Institute of Health Sciences. Bio here
Carl Heneghan is Professor of Evidence-Based Medicine, Director of the Centre for Evidence-Based Medicine and Director of Studies for the Evidence-Based Health Care Programme. (Full bio and disclosure statement here)
Jason Oke is a Senior Statistician at the Nuffield Department of Primary Care Health Sciences and Module Coordinator for Statistical Computing with R and Stata (EBHC Med Stats), and Introduction to Statistics for Health Care Research (EBHC), as part of the Evidence-Based Health Care Programme.
Tom Jefferson is an epidemiologist. Disclosure statement is here.
Disclaimer: the article has not been peer-reviewed; it should not replace individual clinical judgement, and the sources cited should be checked. The views expressed in this commentary represent the views of the authors and not necessarily those of the host institution, the NHS, the NIHR, or the Department of Health and Social Care.

